Pelvic Health Physical Therapy Level 1 Lab
Eligibility Requirements
- Licensed Physical Therapist (PT)
- Licensed Physical Therapist Assistant (PTA)
- 2nd Year Physical Therapy Student (SPT)
- 3rd Year Physical Therapy Student (SPT)
- No other professional types are permitted for this course. No exceptions will be made.
Prerequisites
- Successful completion of the PH1 webinar.
- We recommend students have some orthopedic and musculoskeletal coursework in their curriculum before attending the course.
Overview
Course participants of all genders may be present in the room during the completion of examinations. Please see the requirements regarding lab participation expectations and model instructions.
Topics
- Anatomy of the pelvic girdle
- Physiology of micturition
- Dysfunctions of the lower urinary tract
- Dysfunctions of the pelvic muscles
- Patient history examination
- Testing and treatment interventions for patients with underactive pelvic floor muscle conditions.
- Urogynecologic surgeries
- Medication
- Prevention of pelvic floor dysfunction
Learning Objectives
Examination / Evaluation
- Identify and examine the anatomy of the pelvic girdle
- Describe the function of the lower urinary tract and female pelvic organs.
- Demonstrate proper infection control techniques involved in pelvic floor muscle examination.
- Perform an external evaluation of the female genitalia, verbally identifying bones, ligaments, muscles, and other structures.
- Perform an internal pelvic examination identifying muscles, ligaments, and bony prominences with identification of pelvic floor muscle origins and insertions.
- Demonstrate proper technique in testing muscle strength of the levator ani muscles.
- Demonstrate proper technique in testing for pelvic organ prolapse.
- Demonstrate proper use of handheld EMG biofeedback to assess pelvic floor musculature.
Diagnosis / Prognosis
- Differentiate between underactive pelvic floor muscles and overactive pelvic floor muscles.
- Demonstrate an understanding of bladder tests and measurements (bladder diary, urodynamic testing, pad testing, etc.) used in the differential diagnosis process.
- Demonstrate the ability to compose a care plan, including functional goals, prognosis, and length of care for patients with active pelvic floor conditions.
- Explain red flags related to treatment of the pelvic floor and understand when to refer to another healthcare provider.
- Understand urogynecologic surgeries and their effect on prognosis and pelvic floor muscle dysfunction.
- Understand various medications and their effects on the bowel and bladder and identify how that may affect the prognosis for a patient with pelvic floor muscle dysfunction.
Intervention
- Explain the effects of pelvic floor under activity and proper technique of pelvic muscle exercises for rehabilitative purposes.
- Explain the relationship between the abdominal and pelvic floor muscles concerning activities of daily living.
- Describe the various interventions available to strengthen the patient's muscles with an underactive pelvic floor and clinically explain when and why the multiple interventions might be used.
- Demonstrate proper use of a handheld pelvic floor muscle electrical stimulation unit and explain its appropriate uses for a patient with pelvic floor muscle dysfunction.
- Describe techniques that can be used to train (retrain) the bladder and when each intervention might be used.
Instructor

Erica Holland, PT, DPT
Board-Certified Women's Health Clinical Specialist
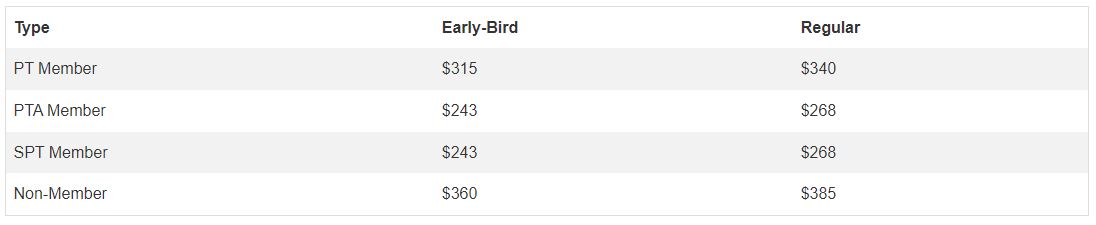
Registration
Des Moines University’s campus, located at 8025 Grand Avenue in West Des Moines, Iowa, offers an impressive 88 acres, providing ample space for growth and innovation. State-of-the-art facilities cater to the evolving needs of students and faculty, fostering an exceptional learning and research environment.
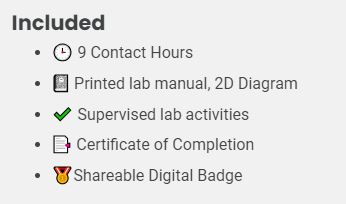
Available Credit
- 9.00 CE Contact Hour(s)

 Facebook
Facebook X
X LinkedIn
LinkedIn Forward
Forward