POSTER ABSTRACTS
Materials should NOT be shared with those that are not registered for the conference. Poster abstracts are not proofed for spelling and/or grammar errors.
The poster and/or other information contained on this website may NOT be downloaded and/or used without prior written permission from all authors on the project. If you would like to be connected with the author(s), please email [email protected].
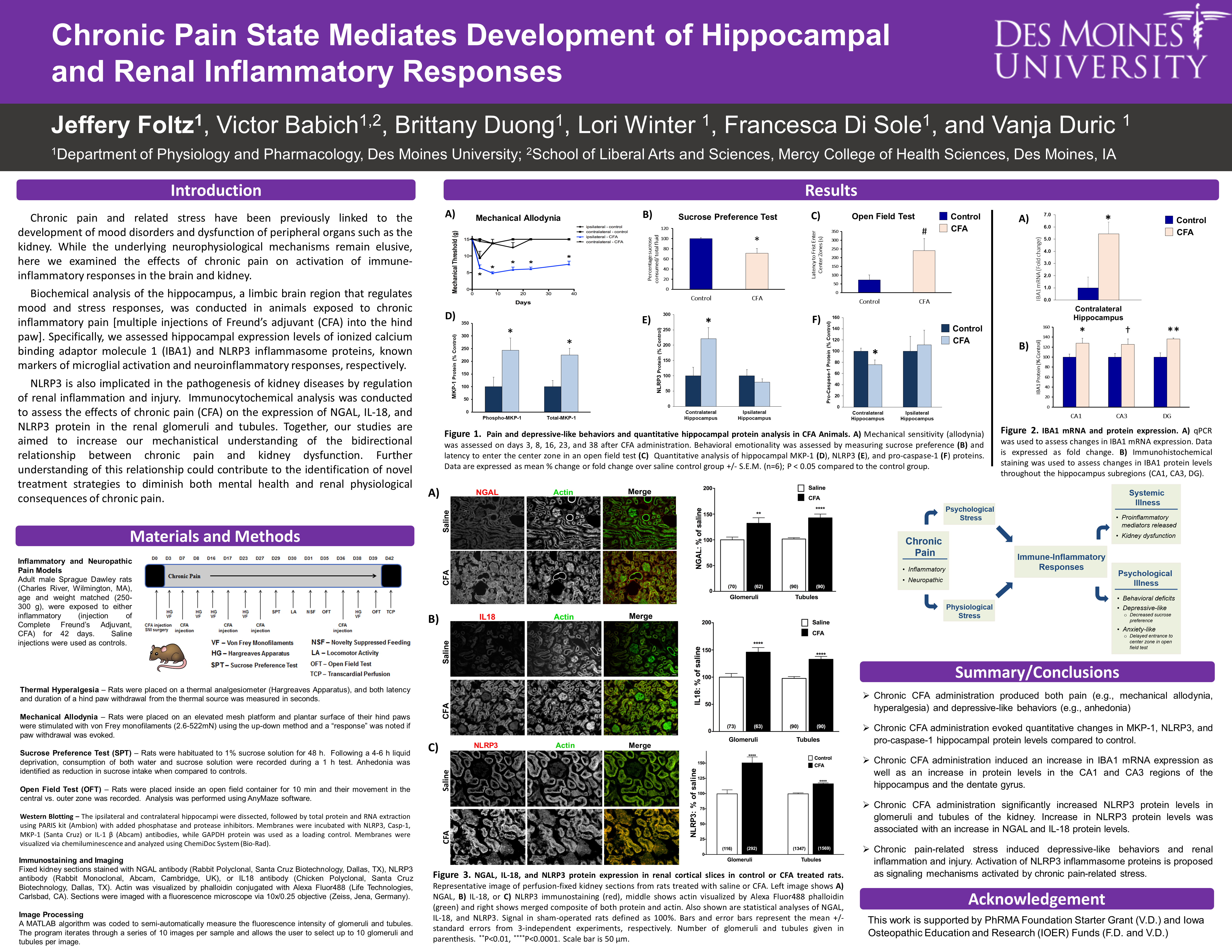
Chronic Pain State Mediates Development of Hippocampal and Renal Inflammatory Responses
1Jeff Foltz, MSBS'22, 1,2Victor Babich, PhD, 1Brittany Duong, 1Lori Winter, 1Francesca Di Sole, PhD, and 1Vanja Duric, PhD
1Department of Physiology and Pharmacology, Des Moines University, Des Moines, IA
2School of Liberal Arts and Sciences, Mercy College of Health Sciences, Des Moines, IA
Abstract
Chronic pain and related stress have been previously linked to the development of mood disorders and dysfunction of peripheral organs such as the kidney. While the underlying neurophysiological mechanisms remain elusive, here we examined the effects of chronic pain on activation of immune-inflammatory responses in the brain and kidney. Male rats were exposed to chronic inflammatory pain for up to 42 days [multiple injections of Freund’s adjuvant (CFA) into the hind paw], which produced a state of chronic allodynia and enhanced behavioral emotionality. Biochemical analysis of the hippocampus, a limbic region that regulates mood and stress responses, showed that CFA evoked increases in expression of ionized calcium binding adaptor molecule 1 (IBA1) and NLRP3 inflammasome proteins, known markers of microglial activation and neuroinflammatory responses, respectively. An increase in the neutrophil gelatinase-associated lipocalin (NGAL) and IL-18 are recognized as early diagnostic injury and inflammatory biomarkers of kidney disease. NLRP3 is implicated in the pathogenesis of kidney diseases by regulation of renal inflammation. Analysis via immunocytochemistry demonstrated that CFA also evoked significant increases in NGAL, IL-18 and NLRP3 protein levels in the renal glomeruli and tubules, suggesting that chronic pain and related stress effects induce renal inflammation and possibly a reduction in kidney function. Together, these findings provide new evidence to support a mechanistical understanding of a bidirectional relationship between chronic pain-related stress and kidney dysfunction. Further understanding of this relationship could contribute to the identification of novel treatment strategies to diminish both mental health and renal physiological consequences of chronic pain.
Key words: chronic pain, hippocampus, kidney, NLRP3, NGAL, IL-18
Support:
- PhRMA Foundation Starter Grant
- Iowa Osteopathic Education and Research Funds
Access PDF version to expand view.