POSTER ABSTRACTS
Materials should NOT be shared with those that are not registered for the conference. Poster abstracts are not proofed for spelling and/or grammar errors.
The poster and/or other information contained on this website may NOT be downloaded and/or used without prior written permission from all authors on the project. If you would like to be connected with the author(s), please email [email protected].
Potential renoprotective effects of chronic remote ischemic conditioning in a rodent model of sleep apnea
1Benjamin G. Madigan, DO'24, 1Katherine Harbeck, DO'24, 1Raina Gerritts, DO'24, 1Kalie A. Savage, 1Sarah C. Clayton, PhD, 1Kiefer W. Kious, MS, 2Kelsey S. Schwartz, 2James A. Lang, PhD, 1Noah J. Marcus, PhD
1Department of Physiology and Pharmacology, College of Osteopathic Medicine, Des Moines University, Des Moines, IA
2Department of Kinesiology, Iowa State University, Ames IA
Abstract
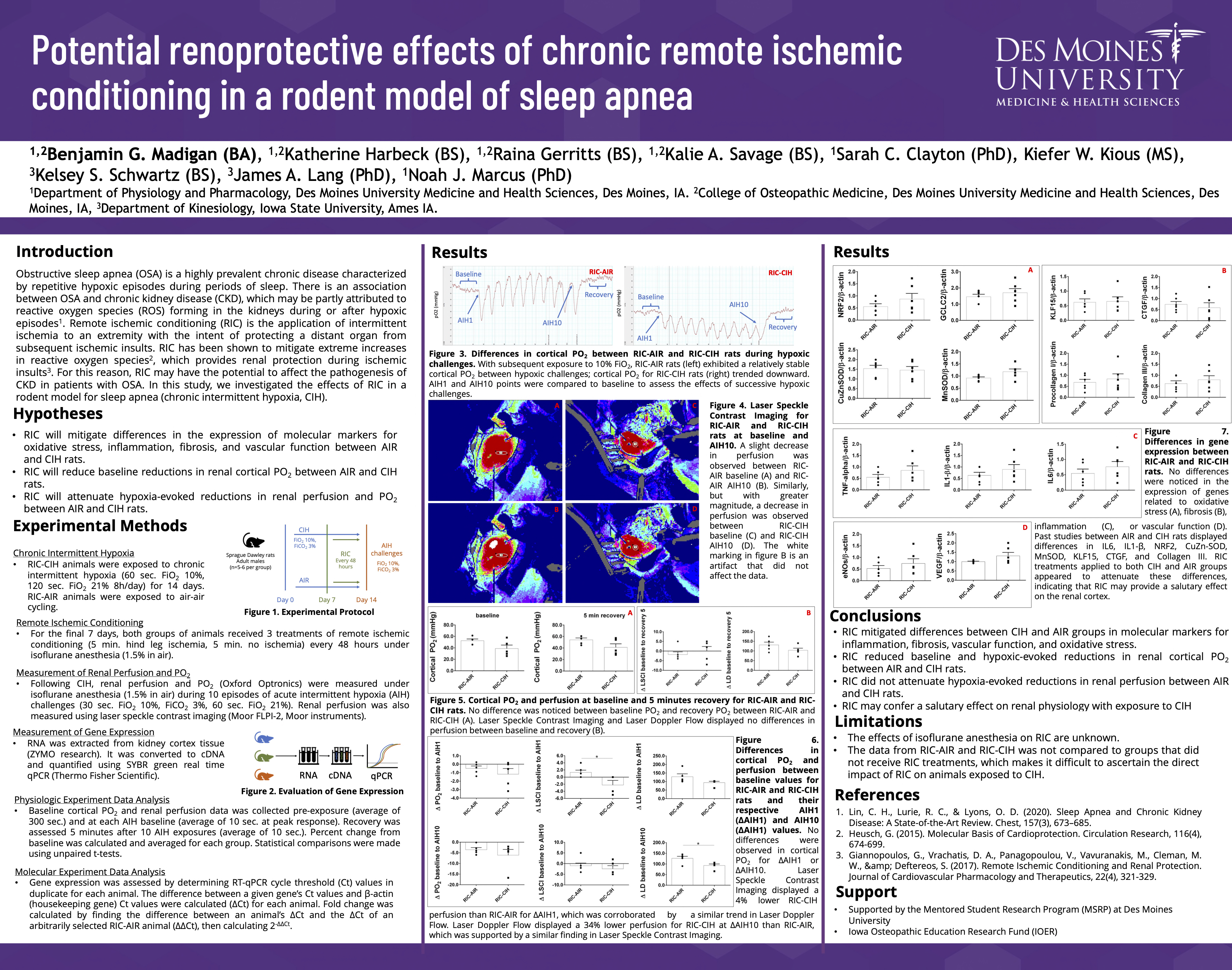
Remote ischemic conditioning (RIC) is the application of intermittent ischemia to an extremity with the intent of protecting a distant organ from subsequent ischemic insults. RIC has been shown to have renoprotective effects in acute settings, however the benefits of RIC in treating chronic illnesses is unknown. Sleep apnea (SA) is a highly prevalent disorder that is associated with chronic kidney disease; therefore, SA patients may benefit from the renoprotective effects of RIC. We hypothesized that the application of RIC in a rodent model of SA (chronic intermittent hypoxia, CIH) would have beneficial effects on the regulation of renal hemodynamics and prevent inflammation, oxidative stress, and pro-fibrotic signaling. Adult male Sprague Dawley rats were exposed to CIH or sham for 14 days; two sub-groups (n=6 per group) received RIC every 48 hours over the final 7 days. Renal perfusion and PO2 were measured at baseline and in response to hypoxia. Cortical tissue was assessed for gene expression related to inflammation, oxidative stress, and fibrosis using qRT-PCR. CIH resulted in baseline reductions in renal blood flow and PO2 relative to sham in addition to greater hypoxia-evoked reductions in these measures(p<0.05). No differences were observed in renal blood flow/perfusion or PO2 between RIC-AIR and RIC-CIH groups (p>0.05). Cortical expression of IL-6, IL-1β, CuZn-SOD, and Collagen III were increased in CIH vs. sham (p<0.05), whereas no differences in expression were observed between RIC-AIR and RIC-CIH groups (p>0.05). These results suggest RIC may confer a salutary effect on renal physiology with exposure to CIH.
Access PDF version to expand view.